Leading US Insurance Company
Back to Home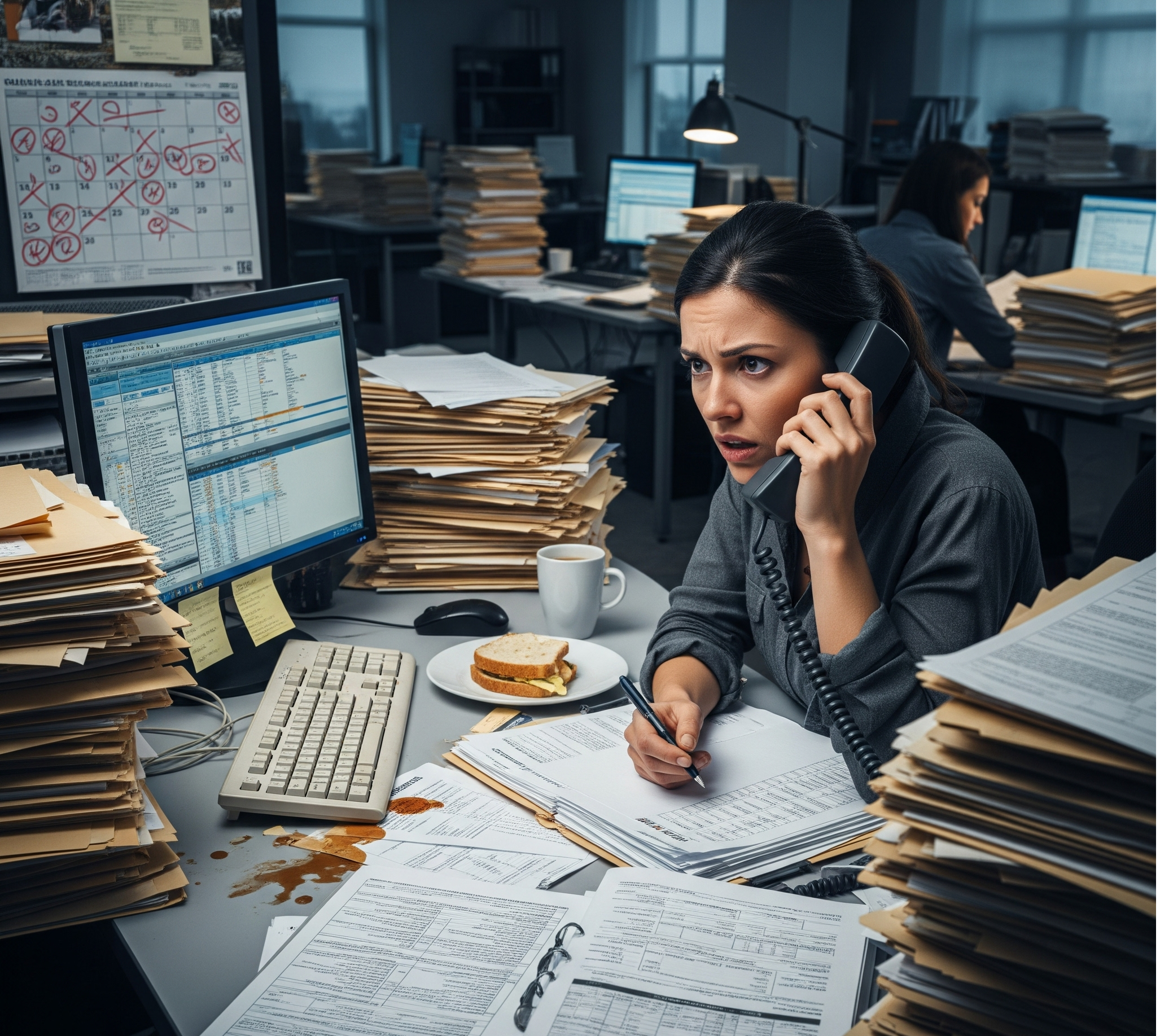
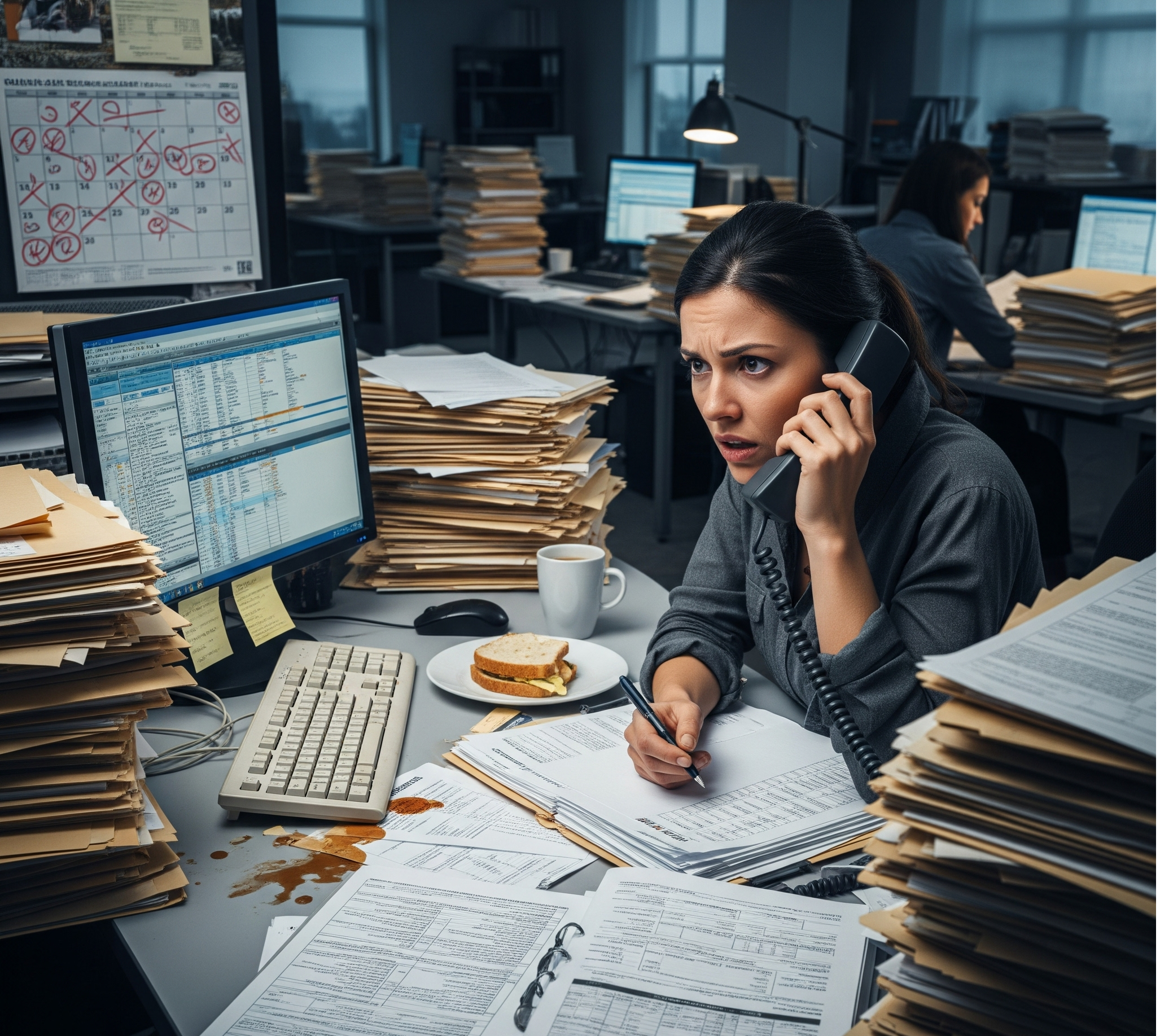
Manual, inefficient FNOL (First Notice of Loss) process led to delays, bad debts, and poor experiences for policyholders and claims handlers.
E2E self-serve Claims STP using AI/NLP/CV, workflow automation, and digital levers for business efficiency and user experience.
Automated claims processing with intelligent decision making
Automated damage assessment and documentation
Advanced algorithms to identify suspicious claims
Straight Through Processing rate achieved
Overall operational efficiency improved
Fraudulent claims detection improved
Average Handling Time significantly reduced
Leading US Insurance Company
Insurance
E2E Claims Automation Platform
8 months